Leads ECG Placement: 7 Critical Mistakes to Avoid Now!
Understanding leads ecg placement is crucial for accurate heart monitoring—get it wrong, and you risk misdiagnosis. This guide reveals the secrets professionals use to ensure precision every time.
What Is Leads ECG Placement and Why It Matters

Leads ecg placement refers to the strategic positioning of electrodes on the body to record the heart’s electrical activity. This process is fundamental in electrocardiography (ECG or EKG), a non-invasive test widely used in clinical settings to assess cardiac function. Proper placement ensures that the electrical signals from the heart are captured accurately, allowing healthcare providers to detect arrhythmias, ischemia, myocardial infarction, and other cardiac abnormalities.
The Science Behind ECG Leads
An ECG works by measuring the voltage differences between electrodes placed on the skin. These voltages reflect the depolarization and repolarization of cardiac muscle cells during each heartbeat. The standard 12-lead ECG uses 10 electrodes—4 on the limbs and 6 on the chest—to generate 12 different ‘views’ or leads of the heart’s electrical activity. Each lead provides a unique perspective, enabling a comprehensive analysis of the heart’s function from multiple angles.
- Lead I measures the electrical activity between the right and left arms.
- Lead II runs from the right arm to the left leg, often used in monitoring during surgery.
- Lead III completes the limb triangle, measuring from the left arm to the left leg.
The augmented limb leads (aVR, aVL, aVF) provide additional views by combining inputs from two limbs and comparing them to the third. Together with the six precordial (chest) leads (V1–V6), they form the complete 12-lead system essential for diagnosing a wide range of cardiac conditions.
“Accurate leads ecg placement is not just a technical detail—it’s the foundation of reliable cardiac diagnosis.” — American Heart Association
Common Misconceptions About Leads ECG Placement
One widespread misconception is that slight deviations in electrode placement do not significantly affect the ECG reading. However, research shows that even small shifts—such as moving a chest electrode by just one intercostal space—can alter the morphology of the ECG, leading to false diagnoses like anterior myocardial infarction or misinterpretation of ST-segment changes.
- Myth: Chest leads can be placed anywhere on the torso as long as they’re roughly in the right area.
- Truth: Precise anatomical landmarks must be followed to ensure consistency and accuracy.
- Myth: Limb leads can be placed on the upper arms and thighs instead of the wrists and ankles without consequence.
- Truth: While acceptable in certain clinical situations (e.g., burns or amputations), improper limb placement can distort waveforms and lead to diagnostic errors.
Another common error is assuming that modern ECG machines can automatically correct for poor lead placement. While some digital systems offer filtering and noise reduction, they cannot compensate for anatomically incorrect electrode positioning. Therefore, human precision remains irreplaceable.
Step-by-Step Guide to Correct Leads ECG Placement
Performing a standard 12-lead ECG requires meticulous attention to detail. Following a standardized protocol ensures reproducibility and diagnostic accuracy. Here’s how to correctly perform leads ecg placement in a clinical setting.
Preparing the Patient and Equipment
Before placing any electrodes, ensure the patient is lying comfortably in a supine position. Expose the chest, wrists, and ankles while maintaining patient privacy. Clean the skin with an alcohol wipe to remove oils, sweat, or dead skin cells that could interfere with conductivity. In patients with excessive chest hair, consider clipping (not shaving) the area to improve electrode adhesion.
- Use high-quality, single-use electrodes to minimize impedance.
- Check the ECG machine for proper calibration and lead integrity.
- Ensure all cables are undamaged and connectors are secure.
Explain the procedure to the patient to reduce anxiety, which can cause muscle tremors and affect the tracing. Ask the patient to remain still and breathe normally during the recording.
Placing Limb Leads Accurately
The four limb electrodes are placed on the right arm (RA), left arm (LA), right leg (RL), and left leg (LL). Although these are often placed on the wrists and ankles, they may be positioned on the upper arms and thighs if necessary, as long as they are placed symmetrically and not over joints.
- RA (White): Right wrist or upper right arm.
- LA (Black): Left wrist or upper left arm.
- RL (Green): Right ankle or lower right leg (ground electrode).
- LL (Red): Left ankle or lower left leg.
The ground electrode (usually green) does not participate in recording but stabilizes the signal. Incorrect placement of limb leads can result in axis deviation, altered P-wave morphology, and misleading ST-segment changes. For example, swapping RA and LA leads can mimic dextrocardia or lead to misinterpretation of ischemic patterns.
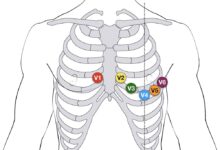
Positioning the Precordial (Chest) Leads
The six chest leads (V1–V6) are placed in specific intercostal spaces along defined anatomical landmarks. Accuracy here is critical because these leads directly reflect anterior, lateral, and septal wall activity.
- V1: 4th intercostal space, right sternal border.
- V2: 4th intercostal space, left sternal border.
- V3: Midway between V2 and V4.
- V4: 5th intercostal space, midclavicular line.
- V5: Same horizontal level as V4, anterior axillary line.
- V6: Same level as V4 and V5, midaxillary line.
Incorrect placement of V1 and V2 too high or too lateral can mimic right bundle branch block or anterior infarction. Placing V4 below the 5th intercostal space—common in women with large breasts—can distort QRS amplitude and lead to false-positive results. Always document any deviations from standard placement in the patient’s record.
Common Errors in Leads ECG Placement and How to Avoid Them
Even experienced clinicians can make mistakes in leads ecg placement. These errors can lead to inaccurate readings, misdiagnoses, and inappropriate treatment. Recognizing and avoiding these pitfalls is essential for high-quality patient care.
Misplacement of Chest Leads
One of the most frequent errors is incorrect placement of the precordial leads. Studies show that up to 50% of ECGs have at least one misplaced chest electrode. V1 and V2 are often placed too high (e.g., in the 2nd or 3rd intercostal space), which can exaggerate R-wave progression and mimic posterior myocardial infarction.
- Solution: Palpate the sternal angle (Angle of Louis) to locate the 2nd rib, then count down to the 4th intercostal space.
- Use anatomical landmarks consistently, not visual estimation.
- Recheck placement before recording, especially in obese or dyspneic patients.
Another common issue is placing V4, V5, and V6 too low, particularly in women. The 5th intercostal space should be identified at the midclavicular line, not estimated from the nipple line, which varies widely in position.
Limb Lead Reversal
Limb lead reversal—especially RA and LA—is surprisingly common. This mistake in leads ecg placement causes dramatic changes in the ECG, including negative P waves in lead I, inverted QRS complexes, and a rightward shift in the electrical axis.
- Right arm/left arm reversal: Causes lead I to invert and mimics dextrocardia.
- Right leg/left leg reversal: Less common but can affect inferior leads (II, III, aVF).
- Arm/leg lead reversal: Can distort limb lead voltages and mimic limb ischemia.
To prevent this, use color-coded electrodes and double-check connections. Many ECG machines now include lead reversal detection algorithms, but these are not foolproof. Always visually confirm placement before initiating the recording.
Failure to Adapt for Special Populations
Standard leads ecg placement guidelines assume a typical adult anatomy. However, modifications are often needed for pediatric, obese, pregnant, or post-surgical patients.
- In women with large breasts, lift the breast tissue to place V3–V6 on the chest wall, not on the breast.
- In pediatric patients, electrode placement follows the same landmarks but may require smaller electrodes.
- In patients with amputations, use alternative sites (e.g., upper arms) and clearly document the modification.
Failure to adapt leads ecg placement for these populations can result in non-diagnostic tracings or false abnormalities. Always tailor the procedure to the individual patient while maintaining anatomical accuracy.
The Impact of Incorrect Leads ECG Placement on Diagnosis
Incorrect leads ecg placement doesn’t just produce a messy tracing—it can directly influence clinical decisions. Misdiagnosis due to technical error is a significant concern in cardiology and emergency medicine.
False Positives and Unnecessary Interventions
A misplaced V1 electrode can create the appearance of a right bundle branch block or anterior ST-elevation myocardial infarction (STEMI). This may trigger unnecessary activation of the cardiac catheterization lab, exposing the patient to invasive procedures, radiation, and contrast agents without clinical benefit.
- Example: A patient with misplaced V1 showed ST elevation in V1–V3, leading to a suspected anterior MI. After repeat ECG with correct placement, the abnormality resolved.
- Cost implications: Unnecessary cardiac interventions can cost thousands of dollars per patient.
Similarly, limb lead reversal can mimic dextrocardia or complex intraventricular conduction delays, prompting further imaging or specialist consultation when none is needed.
False Negatives and Missed Diagnoses
Conversely, incorrect placement can mask real pathology. If V4 is placed too low, ST elevation from an inferior MI may be missed. If chest leads are rotated or misplaced laterally, anterior ischemia might not be detected.
- Case study: A patient with acute chest pain had a ‘normal’ ECG due to V4 placement in the 6th intercostal space. Repeat ECG with proper placement revealed significant ST elevation.
- Delayed treatment: Missed MI can lead to increased mortality and long-term complications like heart failure.
These diagnostic errors underscore the importance of standardized training and quality control in ECG performance.
Legal and Ethical Implications
Inaccurate ECG interpretation due to poor leads ecg placement can have legal consequences. If a misdiagnosis leads to patient harm, it may constitute negligence, especially if proper protocols were not followed.
- Hospitals may face malpractice claims if ECG errors contribute to adverse outcomes.
- Documentation of lead placement is critical for legal defensibility.
- Training and competency assessments for ECG technicians are essential risk management strategies.
Ensuring correct leads ecg placement is not just a technical skill—it’s an ethical obligation to provide safe, accurate, and reliable patient care.
Best Practices for Ensuring Accurate Leads ECG Placement
Consistency, training, and attention to detail are the cornerstones of accurate leads ecg placement. Implementing best practices can significantly reduce errors and improve diagnostic reliability.
Standardized Protocols and Checklists
Hospitals and clinics should adopt standardized ECG protocols based on guidelines from organizations like the American Heart Association (AHA) and the European Society of Cardiology (ESC). These protocols should include step-by-step instructions, anatomical diagrams, and verification steps.
- Use a pre-procedure checklist to confirm electrode type, skin preparation, and lead placement.
- Implement a ‘time-out’ before recording, similar to surgical safety protocols.
- Require dual verification in high-risk settings (e.g., emergency departments).
Checklists have been shown to reduce procedural errors in multiple medical fields, including ECG performance.
Ongoing Training and Competency Assessment
Regular training for nurses, ECG technicians, and medical students is essential. Many errors stem from inadequate initial training or lack of refresher courses.
- Conduct hands-on workshops with mannequins and real-time feedback.
- Use ECG simulators to test lead placement accuracy.
- Perform periodic competency assessments with direct observation.
According to a study published in Circulation, institutions with structured ECG training programs reported a 40% reduction in lead placement errors.
Use of Technology and Verification Tools
Modern ECG machines often include features to detect lead reversals and poor signal quality. While not a substitute for proper technique, these tools can serve as a safety net.
- Enable lead reversal alerts on the ECG device.
- Use real-time waveform monitoring to detect artifacts before recording.
- Consider digital ECG systems with placement guidance overlays.
Some advanced systems use augmented reality or camera-based guidance to assist with electrode placement, particularly in complex cases. These innovations hold promise for improving accuracy in the future.
Special Considerations in Leads ECG Placement
While standard leads ecg placement works for most patients, special populations require tailored approaches to ensure diagnostic accuracy.
Leads ECG Placement in Women
One of the most challenging aspects of leads ecg placement is managing ECGs in women, particularly those with large or ptotic breasts. Placing V3–V6 on the breast tissue rather than the chest wall can dampen electrical signals and distort waveforms.
- Always lift the breast to place electrodes on the rib cage.
- Use extra adhesive or support straps if needed.
- Document any modifications in the patient’s chart.
A study in the Journal of the American Medical Association (JAMA Internal Medicine) found that up to 30% of ECGs in women had incorrect V-lead placement due to breast interference.
ECG in Pediatric and Neonatal Patients
Children have smaller body sizes and different proportions, requiring adjustments in leads ecg placement. However, the anatomical landmarks remain the same.
- Use pediatric-sized electrodes to ensure good contact.
- Place V4 at the 5th intercostal space in the midclavicular line, even in infants.
- Ensure limb leads are placed on the limbs, not the trunk, to avoid signal distortion.
In neonates, the right ventricle is more dominant, so the ECG shows a rightward axis and prominent R waves in V1—this is normal and should not be mistaken for pathology.
ECG in Obese and Post-Surgical Patients
Obesity can make anatomical landmarks difficult to palpate, increasing the risk of misplaced leads. In post-mastectomy patients, chest lead placement may need to be adjusted.
- Use ultrasound guidance in morbidly obese patients to locate intercostal spaces.
- In mastectomy patients, place electrodes in the same anatomical position, noting the absence of breast tissue.
- Avoid placing chest leads over surgical scars or drains.
Clear documentation of any deviations is essential for accurate interpretation and comparison with future ECGs.
Future Innovations in Leads ECG Placement
As technology advances, new tools are emerging to improve the accuracy and efficiency of leads ecg placement, reducing human error and enhancing patient outcomes.
Wearable ECG Devices and Smart Electrodes
Wearable ECG monitors, such as the Zio Patch or Apple Watch ECG, are changing how cardiac data is collected. While these devices use fewer leads, they rely on precise sensor placement for reliable readings.
- Smart electrodes with built-in sensors can confirm correct anatomical positioning.
- Bluetooth-enabled patches provide continuous monitoring with automatic placement validation.
- AI algorithms analyze signal quality in real time and alert users to reposition sensors.
These innovations are particularly useful for ambulatory monitoring and remote patient management.
Augmented Reality and AI Guidance
Researchers are developing augmented reality (AR) systems that overlay anatomical landmarks on a patient’s body using a tablet or smart glasses. This technology guides clinicians to the exact placement points for each lead.
- AR systems reduce reliance on estimation and improve first-time accuracy.
- AI-powered cameras can detect electrode position and suggest corrections.
- Integration with EHR systems allows automatic documentation of placement technique.
A pilot study at Stanford University showed a 60% reduction in lead placement errors when AR guidance was used.
Standardization and Global Protocols
There is growing momentum toward global standardization of leads ecg placement. Organizations like the International Society for Computerized Electrocardiology are working on unified guidelines to reduce variability across countries and institutions.
- Universal color-coding and labeling standards.
- Standardized training curricula for healthcare providers.
- Global certification programs for ECG technicians.
Such efforts could dramatically improve the reliability of ECG data in research, telemedicine, and cross-border patient care.
What happens if ECG leads are placed incorrectly?
Incorrect leads ecg placement can lead to misdiagnosis, including false positives for heart attacks or false negatives that miss real cardiac events. It can also trigger unnecessary tests, increase patient anxiety, and result in inappropriate treatment.
Can limb leads be placed on the upper arms and thighs?
Yes, limb leads can be placed on the upper arms and thighs if necessary (e.g., due to wounds or amputations), but they must be placed symmetrically and not over joints. However, placement on the wrists and ankles is preferred for consistency.
How do you ensure accurate chest lead placement in women?
Lift the breast tissue to place V3–V6 directly on the chest wall at the correct intercostal spaces. Never place electrodes on the breast itself, as this can distort the ECG signal and lead to inaccurate results.
Are there tools to detect ECG lead reversal?
Yes, many modern ECG machines have built-in algorithms that detect common lead reversals (e.g., RA/LA swap). However, these tools are not 100% reliable, so visual confirmation of lead placement remains essential.
What is the most common ECG lead placement error?
The most common error is misplacement of the precordial leads, especially V1 and V2, which are often placed too high. Limb lead reversal, particularly of the right and left arms, is also frequent and can significantly alter the ECG tracing.
Accurate leads ecg placement is a critical skill that directly impacts patient diagnosis and care. From understanding the anatomy to avoiding common errors and embracing future innovations, every step matters. By following standardized protocols, investing in training, and leveraging new technologies, healthcare providers can ensure reliable, high-quality ECGs that support accurate clinical decisions.
Further Reading: